Introduction
The pathophysiology of diabetes mellitus is a multifaceted journey, involving intricate mechanisms that disrupt the body’s ability to regulate blood sugar levels. This comprehensive guide aims to unravel the complexities of diabetes mellitus, exploring its various types, underlying causes, and the physiological processes that contribute to this prevalent metabolic disorder.
Step 1: Understanding the Basics of Diabetes Mellitus Embark on the journey by understanding the fundamental aspects of diabetes mellitus, a chronic condition characterized by elevated blood glucose levels. This section provides a concise overview of the two primary types: Type 1 diabetes, an autoimmune disorder, and Type 2 diabetes, associated with insulin resistance.
Step 2: Beta Cell Dysfunction in Type 1 Diabetes Delve into the pathophysiology of Type 1 diabetes, where the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. This autoimmune response results in an absolute insulin deficiency, disrupting glucose metabolism and leading to elevated blood sugar levels.
Step 3: Insulin Resistance in Type 2 Diabetes Explore the mechanisms underlying Type 2 diabetes, primarily characterized by insulin resistance. This section outlines how cells become less responsive to insulin, impairing glucose uptake, and prompting the pancreas to compensate by producing more insulin. Over time, beta cell exhaustion can occur, contributing to elevated blood glucose levels.
Step 4: Role of Insulin in Glucose Regulation Understand the pivotal role of insulin in glucose regulation. Insulin acts as a key that unlocks cells, allowing glucose to enter and be utilized for energy. In diabetes, whether due to autoimmune destruction (Type 1) or resistance (Type 2), this process is disrupted, resulting in elevated blood sugar levels.
Step 5: Impact on Organs and Systems Examine the widespread impact of diabetes mellitus on various organs and systems. Chronic hyperglycemia can lead to complications affecting the eyes (diabetic retinopathy), kidneys (diabetic nephropathy), nerves (diabetic neuropathy), and cardiovascular system (increased risk of heart disease and stroke), highlighting the systemic nature of the disorder.
Additional Information
- Glycemic Dysregulation: Provide insights into glycemic dysregulation, elucidating how the disruption of insulin and glucose balance can lead to fluctuations in blood sugar levels, contributing to both acute and chronic complications.
- Lifestyle Factors and Genetics: Explore the influence of lifestyle factors, such as diet and physical activity, and genetic predispositions in the development and progression of diabetes mellitus, emphasizing the importance of a holistic approach to prevention and management.
- Emerging Therapies: Briefly touch upon emerging therapies and research endeavors aimed at addressing the pathophysiology of diabetes mellitus, including advancements in insulin delivery systems, glucose monitoring technologies, and targeted medications.
By navigating through these steps and additional information, individuals can gain a comprehensive understanding of the pathophysiology of diabetes mellitus, empowering them to comprehend the underlying processes, make informed lifestyle choices, and work collaboratively with healthcare professionals for effective management of this intricate metabolic disorder.
Pathophysiology
Diabetes Mellitus has different courses of pathophysiology because of it has several types
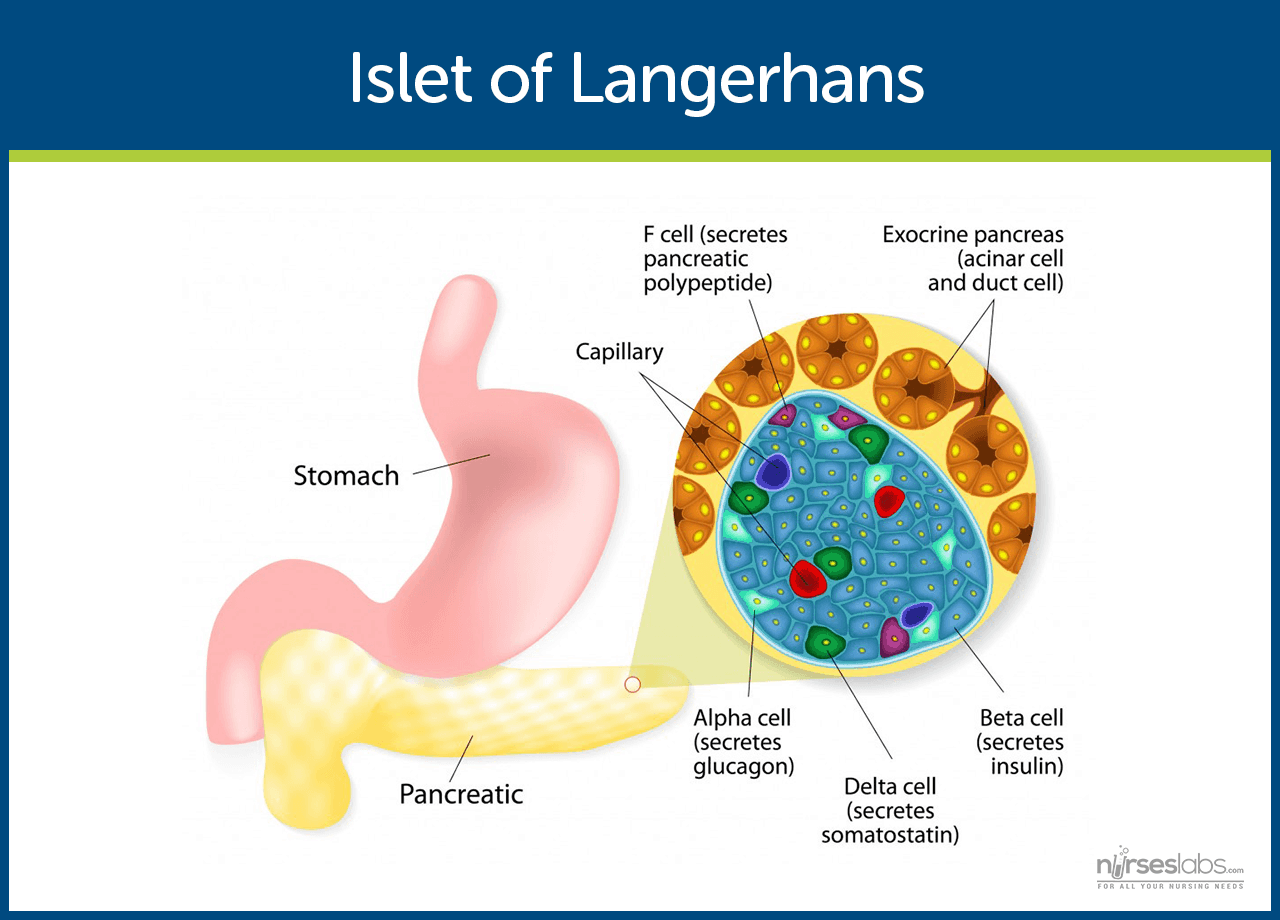
- Insulin is secreted by beta cells in the pancreas and it is an anabolic hormone.
- When we consume food, insulin moves glucose from blood to muscle, liver, and fat cells as insulin level increases.
- The functions of insulin include the transport and metabolism of glucose for energy, stimulation of storage of glucose in the liver and muscle, serves as the signal of the liver to stop releasing glucose, enhancement of the storage of dietary fat in adipose tissue, and acceleration of the transport of amino acid into cells.
- Insulin and glucagon maintain a constant level of glucose in the blood by stimulating the release of glucose from the liver.
Type 1 Diabetes Mellitus
- Type 1 diabetes mellitus is characterized by destruction of the pancreatic beta cells.
- A common underlying factor in the development of type 1 diabetes is a genetic susceptibility.
- Destruction of beta cells leads to a decrease in insulin production, unchecked glucose production by the liver and fasting hyperglycemia.
- Glucose taken from food cannot be stored in the liver anymore but remains in the blood stream.
- The kidneys will not reabsorb the glucose once it has exceeded the renal threshold, so it will appear in the urine and be called glycosuria.
- Excessive loss of fluids is accompanied by excessive excretion of glucose in the urine leading to osmotic diuresis.
- There is fat breakdown which results in ketone production, the by-product of fat breakdown.
Type 2 Diabetes Mellitus
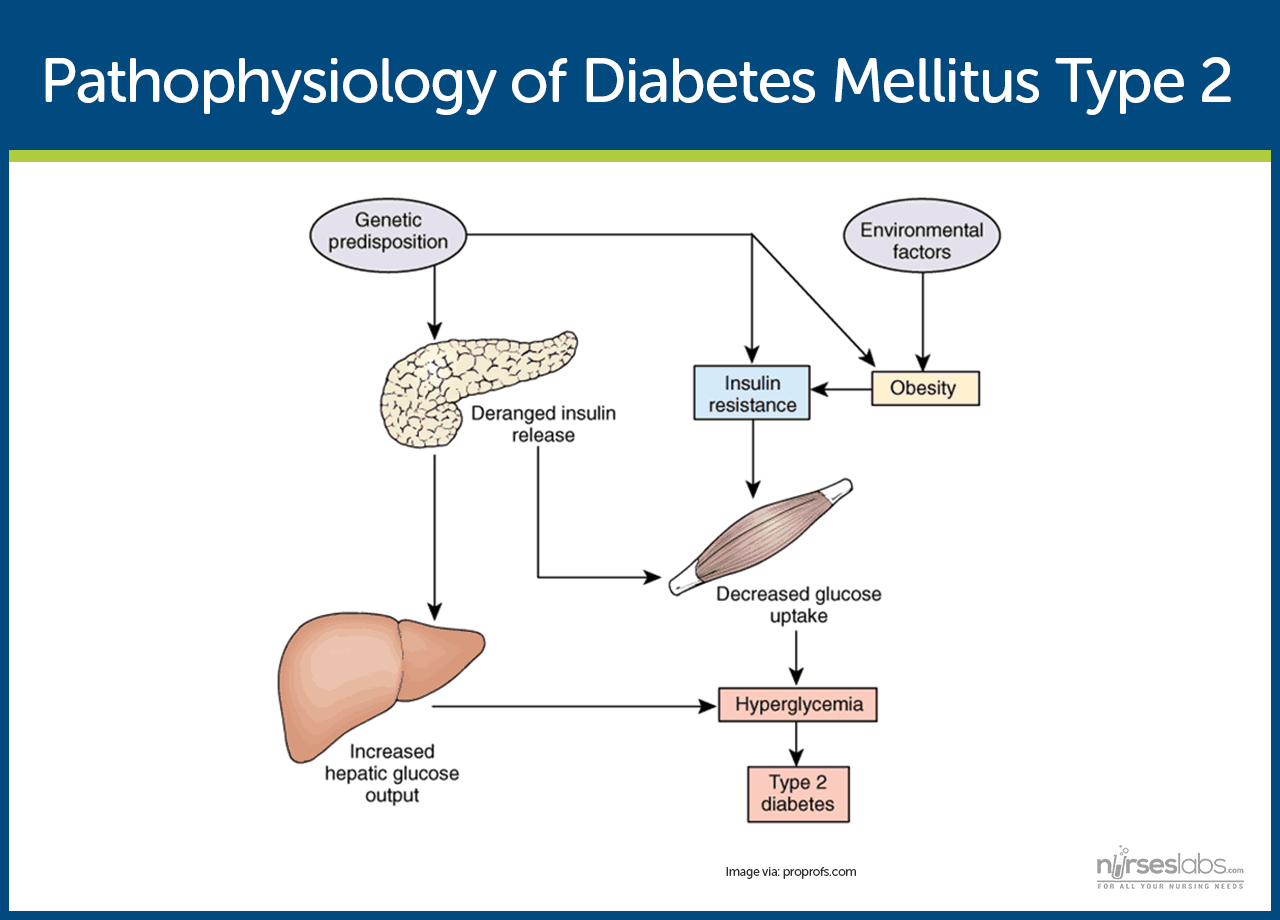
- Type 2 diabetes mellitus has major problems of insulin resistance and impaired insulin secretion.
- Insulin could not bind with the special receptors so insulin becomes less effective at stimulating glucose uptake and at regulating the glucose release.
- There must be increased amounts of insulin to maintain glucose level at a normal or slightly elevated level.
- However, there is enough insulin to prevent the breakdown of fats and production of ketones.
- Uncontrolled type 2 diabetes could lead to hyperglycemic, hyperosmolar nonketotic syndrome.
- The usual symptoms that the patient may feel are polyuria, polydipsia, polyphagia, fatigue, irritability, poorly healing skin wounds, vaginal infections, or blurred vision.
Gestational Diabetes Mellitus
- With gestational diabetes mellitus (GDM), the pregnant woman experiences any degree of glucose intolerance with the onset of pregnancy.
- The secretion of placental hormones causes insulin resistance, leading to hyperglycemia.
- After delivery, blood glucose levels in women with GDM usually return to normal or later on develop type 2 diabetes.
Epidemiology
Diabetes mellitus is now one of the most common disease all over the world. Here are some quick facts and numbers on diabetes mellitus.
- More than 23 million people in the United States have diabetes, yet almost one-third are undiagnosed.
- By 2030, the number of cases is expected to increase more than 30 million.
- Diabetes is especially prevalent in the elderly; 50% of people older than 65 years old have some degree of glucose intolerance.
- People who are 65 years and older account for 40% of people with diabetes.
- African-Americans and members of other racial and ethnic groups are more likely to develop diabetes.
- In the United States, diabetes is the leading cause of non-traumatic amputations, blindness in working-age adults, and end-stage renal disease.
- Diabetes is the third leading cause of death from disease.
- Costs related to diabetes are estimated to be almost $174 billion annually.
Causes
The exact cause of diabetes mellitus is actually unknown, yet there are factors that contribute to the development of the disease.
Type 1 Diabetes Mellitus
- Genetics. Genetics may have played a role in the destruction of the beta cells in type 1 DM.
- Environmental factors. Exposure to some environmental factors like viruses can cause the destruction of the beta cells.
Type 2 Diabetes Mellitus
- Weight. Excessive weight or obesity is one of the factors that contribute to type 2 DM because it causes insulin resistance.
- Inactivity. Lack of exercise and a sedentary lifestyle can also cause insulin resistance and impaired insulin secretion.
Gestational Diabetes Mellitus
- Weight. If you are overweight before pregnancy and added extra weight, it makes it hard for the body to use insulin.
- Genetics. If you have a parent or a sibling who has type 2 DM, you are most likely predisposed to GDM.
Clinical Manifestations
Clinical manifestations depend on the level of the patient’s hyperglycemia.
- Polyuria or increased urination. Polyuria occurs because the kidneys remove excess sugar from the blood, resulting in a higher urine production.
- Polydipsia or increased thirst. Polydipsia is present because the body loses more water as polyuria happens, triggering an increase in the patient’s thirst.
- Polyphagia or increased appetite. Although the patient may consume a lot of food but glucose could not enter the cells because of insulin resistance or lack of insulin production.
- Fatigue and weakness. The body does not receive enough energy from the food that the patient is ingesting.
- Sudden vision changes.The body pulls away fluid from the eye in an attempt to compensate the loss of fluid in the blood, resulting in trouble in focusing the vision.
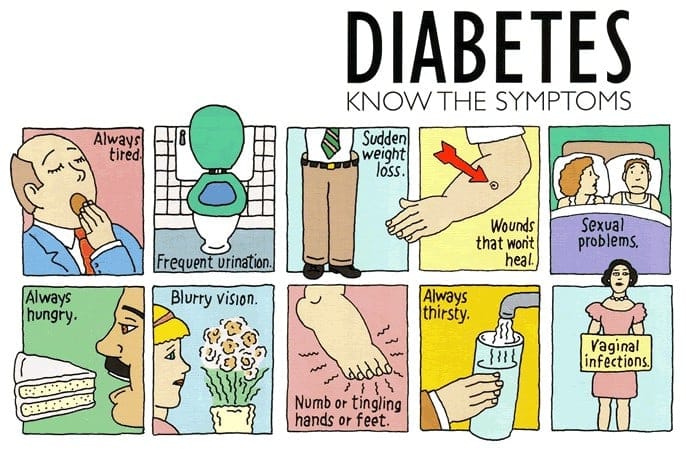
- Tingling or numbness in hands or feet. Tingling and numbness occur due to a decrease in glucose in the cells.
- Dry skin. Because of polyuria, the skin becomes dehydrated.
- Skin lesions or wounds that are slow to heal. Instead of entering the cells, glucose crowds inside blood vessels, hindering the passage of white blood cells which are needed for wound healing.
- Recurrent infections. Due to the high concentration of glucose, bacteria thrives easily.
Prevention
Appropriate management of lifestyle can effectively prevent the development of diabetes mellitus.
- Standard lifestyle recommendations, metformin, and placebo are given to people who are at high risk for type 2 diabetes.
- The 16-lesson curriculum of the intensive program of lifestyle modifications focused on weight reduction of greater than 7% of initial body weight and physical activity of moderate intensity.
- It also included behavior modification strategies that can help patients achieve their weight reduction goals and participate in exercise.
Complications
If diabetes mellitus is left untreated, several complications may arise from the disease
- Hypoglycemia. Hypoglycemia occurs when the blood glucose falls to less than 50 to 60 mg/dL because of too much insulin or oral hypoglycemic agents, too little food, or excessive physical activity.
- Diabetic Ketoacidosis. DKA is caused by an absence or markedly inadequate amounts of insulin and has three major features of hyperglycemia, dehydration and electrolyte loss, and acidosis.
- Hyperglycemic Hyperosmolar Nonketotic Syndrome. HHNS is a serious condition in which hyperosmolarity and hyperglycemia predominate with alteration in the sense of awareness.
Assessment and Diagnostic Findings
Hypoglycemia may occur suddenly in a patient considered hyperglycemic because their blood glucose levels may fall rapidly to 120 mg/dL or even less.
- Serum glucose: Increased 200–1000 mg/dL or more.
- Serum acetone (ketones): Strongly positive.
- Fatty acids: Lipids, triglycerides, and cholesterol level elevated.
- Serum osmolality: Elevated but usually less than 330 mOsm/L.
- Glucagon: Elevated level is associated with conditions that produce (1) actual hypoglycemia, (2) relative lack of glucose (e.g., trauma, infection), or (3) lack of insulin. Therefore, glucagon may be elevated with severe DKA despite hyperglycemia.
- Glycosylated hemoglobin (HbA1C): Evaluates glucose control during past 8–12 wk with the previous 2 wk most heavily weighted. Useful in differentiating inadequate control versus incident-related DKA (e.g., current upper respiratory infection [URI]). A result greater than 8% represents an average blood glucose of 200 mg/dL and signals a need for changes in treatment.
- Serum insulin: May be decreased/absent (type 1) or normal to high (type 2), indicating insulin insufficiency/improper utilization (endogenous/exogenous). Insulin resistance may develop secondary to formation of antibodies.
- Electrolytes:
- Sodium: May be normal, elevated, or decreased.
- Potassium: Normal or falsely elevated (cellular shifts), then markedly decreased.
- Phosphorus: Frequently decreased.
- Arterial blood gases (ABGs): Usually reflects low pH and decreased HCO3 (metabolic acidosis) with compensatory respiratory alkalosis.
- CBC: Hct may be elevated (dehydration); leukocytosis suggest hemoconcentration, response to stress or infection.
- BUN: May be normal or elevated (dehydration/decreased renal perfusion).
- Serum amylase: May be elevated, indicating acute pancreatitis as cause of DKA.
- Thyroid function tests: Increased thyroid activity can increase blood glucose and insulin needs.
- Urine: Positive for glucose and ketones; specific gravity and osmolality may be elevated.
- Cultures and sensitivities: Possible UTI, respiratory or wound infections.
Medical Management
Here are some medical interventions that are performed to manage diabetes mellitus.
- Normalize insulin activity. This is the main goal of diabetes treatment — normalization of blood glucose levels to reduce the development of vascular and neuropathic complications.
- Intensive treatment. Intensive treatment is three to four insulin injections per day or continuous subcutaneous insulin infusion, insulin pump therapy plus frequent blood glucose monitoring and weekly contacts with diabetes educators.
- Exercise caution with intensive treatment. Intensive therapy must be done with caution and must be accompanied by thorough education of the patient and family and by responsible behavior of patient.
- Diabetes management has five components and involves constant assessment and modification of the treatment plan by healthcare professionals and daily adjustments in therapy by the patient.
Nutritional Management
- The foundations. Nutrition, meal planning, and weight control are the foundations of diabetes management.
- Consult a professional. A registered dietitian who understands diabetes management has the major responsibility for designing and teaching this aspect of the therapeutic plan.
- Healthcare team should have the knowledge. Nurses and other health care members of the team must be knowledgeable about nutritional therapy and supportive of patients who need to implement nutritional and lifestyle changes.
- Weight loss. This is the key treatment for obese patients with type 2 diabetes.
- How much weight to lose? A weight loss of as small as 5% to 10% of the total body weight may significantly improve blood glucose levels.
- Other options for diabetes management. Diet education, behavioral therapy, group support, and ongoing nutritional counselling should be encouraged.
